
SERVICES

At Majestic Tan & Spa we offer a wide variety of services.
We have five different levels of tanning beds including:
SUPER BEDS, BRONZING BEDS, and HOT BEDS.
We have two levels of vertical STAND-UP units as well.
Our beds vary in intensity and maximum exposure times depending
on which bed you choose. They range from 8 minutes maximum
exposure to 20 minutes maximum exposure to satisfy every skin type and every preference.
We also offer UV-FREE tanning in our MYSTIC BOOTH.
CLICK
HERE
NO SPAM - JUST GREAT DISCOUNTS VIA
EMAIL
 CLICK HERE FOR MORE INFORMATION |
 |
We have 4 different levels of Mystic solution to choose from including:
Glow, Light, Medium, and Dark. At Majestic we also offer UV-Activating
Teeth Whitening. Whiten your teeth while getting your perfect tan!
We now offer UV-FREE RED LIGHT THERAPY.
Red light therapy helps to reduce fine lines and wrinkles, and diminish
the appearance of stretch marks in only 3 sessions per week! Come in
today and try it out.
You will be amazed at the results!!!
The cosmetic dermatology’s powerful fear-based marketing message,
which drives millions of customers into their offices, has helped grow
their businesses
by 320%. And the existence of the indoor tanning industry is competitive
to dermatology’s multibillion-dollar phototherapy industry. Consider,
according
to the Journal of the American Academy of Dermatology:

Don’t forget our FORMASTAR BODY WRAP treatment room.
Lose yourself to relaxation, rejuvenation, detoxification,
for an hour while you lie in a comfortable message table & lose up to
1400 calories in the process.
Spray On Tan in Action

Sunshine is free – it has no marketing department for its life-giving
benefits.
If a pharmaceutical company patented and sold sunshine, the
public message we receive
about it would be completely different.
Instead,
the professional indoor tanning community
is the only entity in
a position to challenge the $35 billion
anti-UV industry’s total sun
abstinence messaging.
This explains why indoor tanning is under attack
from this powerful coalition of industries who profit from the
exaggerated and largely
unsubstantiated anti-UV message.

Cosmetic Dermatology
We offer spray tanning in a private booth or custom air brush
In 1993, 873,000 phototherapy sessions were delivered in dermatology
offices
in the U.S. By 1998, sessions had fallen off 94 percent to just 53,000.
The cost of a single phototherapy session – which utilizes indoor
tanning equipment
in a dermatologist’s office – is nearly $100 per session, about 20 times
more than an
indoor tanning session. An estimated 1.5 million indoor tanning clients
today successfully
treat psoriasis in indoor tanning facilities.
If tanning salons were closed, the cosmetic dermatology industry would
gain up to
$5 billion in phototherapy sessions which would be charged to health
insurance companies
and the Medicare system. (According to dermatology's own reports,
psoriasis patients
average 35 sessions per year at an estimated average of $85 per
session.)

The dermatology industry is in a hypocritical position when it comes to
indoor tanning:
According to the phototherapy industry’s own practices, dermatologists
use sun burning
dosages of UV light for the clinical treatment of psoriasis, a non-life
threatening disease.
If any UV exposure were as dangerous as a recent statement from the AAD
claims,
then dermatologists would be guilty of violating their Hippocratic oath
for using UV
in burning dosages to treat purely cosmetic skin conditions.
Melanoma mortality is increasing in men over age 50, but dermatology is
targeting its
anti-sun campaign almost exclusively at women under age 50 – the group
most likely to
visit cosmetic dermatology practices for its services.
The American Academy of Dermatology and other skin-care groups get much
of
their marketing budget directly from the chemical sunscreen industry.
The AAD
receives millions for putting endorsement logos on chemical sunscreen
products – a much-criticized "pay for play" program.

Chemical Sunscreen Industry
Chemical sunscreen is mis-marketed as a daily use product – as a
"fear-based purchase" – designed to be worn 365 days a year (in daily
cosmetics for women) – which has
turned chemical sunscreen into a $5-6 billion business controlled by a
handful of major players. Sunscreen also block as much as 99% of vitamin
D production. Consider:
Sunscreen does not prevent melanoma, according to the U.S. Preventive
Services T
ask Force, which makes policy recommendations for the federal
government,
"The evidence is insufficient to recommend sunscreens for the prevention
of skin cancer."
According to the independent Environmental Working Group – a consumer
watchdog group that has analyzed hundreds of sunscreen ingredients,
"Most sunscreen
chemicals are far from innocuous. In sunlight, some release free
radicals that can damage
DNA and cells, promote skin aging and possibly raise risks for skin
cancer. Some act like estrogen and may disrupt normal hormone signaling
in the body. Others may build
up in the body and the environment."
A 2008 Centers for Disease Control study showed that 97 percent of
Americans have the sunscreen active ingredient oxybenzone in our urine.
This ingredient has been linked
to killing coral reefs, changing the gender in fish and potentially
causing cancer.
Chemical Sunscreen manufacturers are not allowed to advertise that
chemical sunscreen
prevents melanoma. So chemical sunscreen companies pay Dermatology
groups millions of dollars to endorse their product and make that claim
on their behalf. The AAD received an estimated $6-8 million in 2009 to
help misbrand chemical sunscreen as a daily-use product.
The Skin Cancer Foundation is a marketing front group organized by
sunscreen
manufacturers to create a "Skin Cancer Foundation Seal of Approval"
which appears on sunscreen products to convince consumers into thinking
their products prevent melanoma,
which they are not allowed to claim themselves. The SCF website says:
"For adequate
protection against melanoma, non-melanoma skin cancers and photo-aging,
everyone over
the age of six months should use sunscreen daily year-round, in any
weather."

Saying that sunlight is harmful and therefore should be avoided is as
misleading as saying that water causes drowning, and therefore we should
avoid water.
Professional indoor tanning facilities promote balance and educate their
patrons about the potential risks of UV overexposure. Consumers are
required to read and sign consent forms
that include warnings about potential eye damage, photoaging and skin
cancer.
Warning labels are found on every tanning device and almost always in
other general areas. Professional tanning facilities require parental
consent for teenagers who tan even
though most states don't require this measure.
While this serious approach to caution is just good sense, it needs to
be noted that
understanding the risks of UV exposure is not as straightforward as some
suggest.
Consider: Research has not established a "causal" relationship Between
Melanoma and Indoor Tanning.
Melanoma skin cancer is the most aggressive of the three major
categories of skin cancer, accounting for only 5 percent of all skin
cancer cases each year, but responsible for a
majority of skin cancer fatalities (Approximately 8,000 annually).
While melanoma has captured a great deal of public attention in the past
15 years, much of the discussion has been oversimplified in stating that
melanoma is caused by overexposure to sunlight. In fact, the exact
nature of the relationship between melanoma and ultraviolet light
remains unclear, and the mechanism by which the two are related is still
unknown –
which is why some independent dermatology researchers even question
whether
the two are related at all.
While it is believed that melanoma is somehow related to ultraviolet
light exposure,
this relationship is not straight-forward and the photobiology research
community still does not know how it works. That’s because while a
minority of associative survey-studies have
suggested a correlation between UV from indoor tanning and melanoma, no
direct experimental evidence exists to show a causative connection. Even
American Academy of Dermatology spokesperson Dr. James Spencer admits,
"We don’t have direct experimental evidence" connecting indoor tanning
and melanoma.
Melanoma is more common in people who work indoors than in those who
work outdoors, and those who work both indoors and outdoors get the
fewest melanomas. Because this is true, the relationship between
melanoma and sunlight cannot possibly be clear-cut. If it were a
clear-cut relationship, outside workers would have higher incidence than
inside workers. But the opposite is true.
Melanoma most commonly appears on parts of the body that do not receive
regular exposure to sunlight. Again, because this is true, the
relationship between melanoma and sunlight cannot be clear-cut. If it
were, melanomas would appear most often on parts of the body that
receive the most sunlight.
18 of 23 epidemiological studies ever conducted attempting to correlate
indoor tanning and melanoma incidence show no statistically significant
association – including the largest independent study, a 2005
multi-ethnic international European study which reported, "The
relationship between UVR and melanoma is very complex and, despite many
studies on
the topic, remains a controversial issue. Some patterns of sun exposure
may also offer protection, as some studies have suggested that people
with heavy occupational exposure to the sun
exhibit a lower risk for melanoma compared to individuals with
intermittent sun exposure.
In conclusion, sunbed and sun exposure were not found to be significant
risk factors for melanoma in this case–control study performed in five
European countries."
A 2009 opinion paper published by an ad-hoc working group representing
the World Health Organization’s International Agency for Research on
Cancer has been widely misrepresented in the media. That report’s actual
conclusion stated, "Epidemiologic studies to date give no consistent
evidence that use of indoor tanning facilities in general is associated
with the development of melanoma or skin cancer." While the report
attempted to suggest that
performing a meta-analysis of the old data showed a 75 percent increased
risk for those
who started tanning at an early age, the authors failed to disclose that
conclusion failed to take into account that removing those with skin so
fair it cannot tan – called Skin Type I –
from the analysis made the overall results statistically insignificant.
Dr. William Grant, founder of the Sunlight, Nutrition and Health
Research Center in San Francisco, published a peer-reviewed critique of
the IARC report showing that, after adjusting for skin type, the
analysis showed no increased risk with indoor tanning.
Closer analysis of IARC report data (by Dr. Mia Papas and Dr. Anne
Chappelle) –
when separated by unsupervised home tanning equipment verses usage in
indoor tanning
facilities and medical usage of tanning equipment in doctor’s offices –
reveals that no
statistically significant increase in risk (6 percent) was attributable
to commercial tanning facility usage, while larger increases (40 percent
and 96 percent) were attributable to home
and medical usage of tanning equipment.
A 2010 University of Minnesota study on fair-skinned Minnesotans claimed
to show a
connection between tanning and melanoma but actually supported Grant’s
point that
UV-related risk seems centered on the fairest skin type. But the study
also showed that those
who got the most outdoor sun exposure had the lowest risk of melanoma –
a divergent
conclusion to the rest of the paper underscoring that whatever
relationship
UV and melanoma may have is still not understood.
The relative risk of melanoma is very small – much less than 1 percent
and very close to the relative risk for non-tanners – and is often
misreported. As reported in the Wilmington News Journal, "Even the
IARC’s strongest study – which followed more than 100,000 women over
eight years – found that less than three-tenths of one percent who
tanned frequently developed melanoma, while less than two-tenths of one
percent who didn’t tan developed melanoma. Almost all the other studies
in the report did not establish a strong link between the two. The
overall risk of contracting melanoma – whether using tanning beds or not
– remains well
under 1 percent. For that reason, using the 75 percent statistic is
misleading, said Dr. Lisa M. Schwartz, general internist at Veterans
Affairs Medical Center in VT and co-author of "Know Your Chances," a
book on understanding health statistics..."Melanoma is pretty rare and
almost all the time, the way to make it look scarier is to present the
relative change, the 75 percent increase, rather than to point out that
it is still really rare."
"Absolute risk just tells you the chance of something happening, while
relative risk tells
you how that risk compares to another risk, as a ratio. If a risk
doubles, for example, that’s
a relative risk of 2, or 200 percent. If it halves, it’s .5, or 50
percent. Generally, when you’re dealing with small absolute risks, as we
are with melanoma, the relative risk differences will seem much greater
than the absolute risk differences. You can see how if someone is
lobbying
to ban something – or, in the case of a new drug, trying to show a
dramatic effect – they would probably want to use the relative
risk."-Ivan Oransky, M.D.
The American Cancer Society’s key document measuring cancer rates in the
United States – "Cancer Facts and Figures" – says that melanoma rates
have not increased since 2000 and that rates are declining for women
under age 50 - the opposite of what anti-tanning lobbying groups claim.
"During the 1970's, the incidence rate of melanoma increased rapidly by
about 6 percent per year. However, from 1981-2000, the rate of increase
slowed to 3 percent per year and since 2000 melanoma incidence has been
stable," the ACS "Cancer Facts and Figures 2008" reports. "The death
rate for melanoma has been decreasing rapidly in whites younger than 50,
by 3 percent per year since 1991 in men and by 2.3 percent per year
since 1985 in women."
A paper published by the British dermatology community in 2009 showed
that
"diagnostic drift" and more aggressive screening are responsible for the
increase in "reported" melanomas, but that there isn’t an actual
increase in thick melanoma lesions, which explains
why the mortality rate is not increasing. According to the authors,
"These findings should lead
to a reconsideration of the treatment of ‘early’ lesions, a search for
better diagnostic methods
to distinguish them from truly malignant melanomas, re-evaluation of the
role of ultraviolet radiation and recommendations for protection from
it, as well as the need for a new direction
in the search for the cause of melanoma.
Many scientists and dermatologists have taken firm positions that
melanoma's connection to UV light is unclear or doesn't exist at all. Dr
Bernard Ackerman – a pioneer in dermatology pathology who was recognized
as a master dermatologist by the American Academy of Dermatology – the
Academy’s highest honor – insists there is no evidence connecting UV and
melanoma in his monograph, "The Sun and the Epidemic of Melanoma: Myth
on Myth. According to Ackerman:
"The American Academy of Dermatology, for decades, has kept up a
drumbeat on behalf of faith in an epidemic of melanoma and rays of the
sun as the major cause of it, at the same time that it has flayed,
incessantly, the tanning bed industry. Although the organization is
termed an Academy, never has it presented in fashion academic a whit of
evidence, available readily, contrary to its position entrenched,
namely, there is no epidemic of melanoma and that tanning beds have not
been proven to be a cause direct of melanoma."
"There is no proof whatsoever that blistering sun-burns, no matter the
number and even in childhood, enhance risk for development of melanoma
and there is no evidence at all that sunscreens prevent development of
melanoma. What is more, it has yet to be established that exposure
excessive to sunlight (or sun lamps and tanning beds) alone, in the
absence of inclination genetic, causes melanoma."
Dr. Sam Shuster, Emeritus Professor of Dermatology at the University of
Newcastle, penned "The Skin Cancer Cover-Up" to point out that there is
no hard evidence that UV is the cause of melanoma or that there is an
actual increase in melanoma incidence.
Dr. Arthur R. Rhodes, Professor of Dermatology at Rush Medical College,
in Chicago, believes that melanoma’s public message needs to stop
focusing on UV light – pointing out that UV-melanoma campaigns are
killing people who get melanoma who failed to recognize the disease
because they never spent time in the sun.
UV Light Does Not Deserve the Blanket Label of 'Carcinogen'
The U.S. National Institutes of Health’s National Toxicology Program in
2000 placed
ultraviolet light on the federal government’s list of known human
carcinogens. In July 2009
the World Health Organization wrote a brief report also declaring that
UV light is a Class I carcinogen – a list that also includes red wine,
birth control pills, salted fish and other highly used substances that,
when experienced in their intended dosages, do not elevate cancer risk.
Much like the NIH listing in 2000, WHO erred in not pointing out that
the "list" doesn't mean a substance is dangerous in every-day dosages,
but only potentially in "overexposure" situations.
The listing does not mean that moderate tanning will cause skin cancer.
The NIH listing criteria shows us why: "The Report does not present
quantitative assessments of carcinogenic risk.
Listing of substances in the Report, therefore, does not establish that
such substances present carcinogenic risks to individuals in their daily
lives." This exclusion – in the absence of any
direct experimental research on indoor tanning and melanoma –
makes this listing almost meaningless.
The list does not take into account that there are positive effects to
ultraviolet light exposure. Many forms of cancer – including breast,
colon, prostate and ovarian tumors – now appear to
be retarded or even prevented by regular exposure to ultraviolet light.
This omission on the NTP list is conspicuous, given that positive
effects are listed for other substances in the government's list of
carcinogens that have positive effects, such as the breast cancer drug
Tamoxifen,
which is a Class I carcinogen.
As a result, thousands of news reports suggest that "sun tanning is as
dangerous as tobacco" –
a blatant misrepresentation.
Smoker’s risk of lung cancer: 15 percent – or 2,000 percent higher than
that of non-smokers. Smoking introduces up to 60 man-made known
carcinogens into the body – substances the body was never designed to
process. Smoking is related to 1 in 3 cancer deaths.
Tanner’s risk of melanoma: 0.3 percent – compared to 0.2 percent for
non-tanners
(a difference of 1 in 1,000) The body needs ultraviolet light to survive
– calling it a
carcinogen without that caveat is totally misleading.
One thing we know for certain: You would be dead today if you did not
receive any ultraviolet light.
Indoor tanning equipment, like outdoor sunlight, emits UVA (ultraviolet
A) and UVB
(ultraviolet B) light. Of the UV light emitted by the sun at noon in the
summer in the United States: 95 percent is UVA and 5 percent is UVB.

More than 90 percent of professional indoor tanning units emit about 95
percent UVA and 5 percent UVB in regulated dosages similar to summer
sun. Recommended exposure schedules developed by the U.S. FDA in
cooperation with the tanning industry allow trained indoor tanning
operators to set incremental exposure times, based on the "skin type" of
a patron, that deliver consistent non-burning dosages of UV light to
allow a tanner to gradually build a tan.
The statement that "indoor tanning units are more intense than sunlight"
is misleading and inaccurate because the total output of a tanning unit
is measured the following way:
Total UV Output = UV Intensity x Duration of Exposure
While tanning units may be 2-3 times as intense as summer sun, the
duration of exposure is controlled, and thus the total UV output is
controlled, to minimize the risk of sunburn. Exposure times in the more
intense tanning units are calculated in similar fashion.
A typical indoor tanning exposure schedule (below) allows a professional
indoor tanning operator to gradually increase the exposure times of a
tanner over the course of the tanner’s regimen based on the individual’s
skin type.
Recommended Exposure Schedule
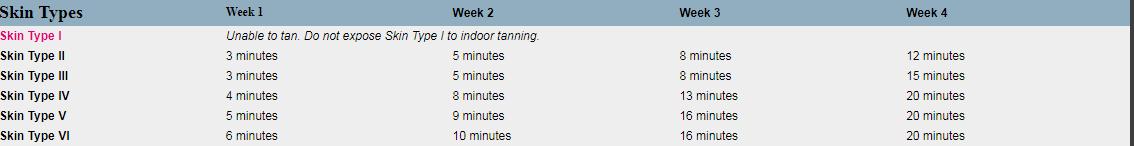
Less than 5 percent of North Americans are what is called
"Skin Type I" – which includes people of Northern
European heritages (some Irish or English people, for example) whose
skin is so fair that it cannot tan without burning. North American
indoor tanning protocol is not to allow these people to tan in salons,
and our skin type questionnaire identifies them. If they wish to tan,
they are advised to use non-UV self-tanning products.
In professional North American tanning facilities today:
1. Trained operators control all tanning exposure times, minimizing a
client’s risk of overexposure and sunburn, and require tanners to use
FDA-compliant protective eyewear,
which eliminates the risk of eye injury.
All clients undergo comprehensive evaluations, including identifying
their sun sensitivity
(skin type). Clients also are taught about photosensitizing medications,
which can potentially make a person more susceptible to sunburn.
Clients are taught sunburn prevention and the appropriate use of outdoor
sunscreen.
Combined with the fact that a tan is nature’s protection against
sunburn, this is why indoor tanning clients are up to 81 percent less
likely to sunburn outdoors as compared to
non-tanners, according to Smart Tan surveys.
Clients are presented with material outlining the potential risks of
overexposure to
UV light and sign informed consent agreements acknowledging this.
Because of all these safeguards, the professional indoor tanning has an
exemplary
safety record: From an estimated 6 billion indoor tanning sessions from
1985-2006
only 142 adverse events are reported in U.S. federal records – most
occurring before 1997. That’s an injury rate of 0.0000000236 – or less
than one report in every 44 million
sessions over a 21-year period, with most of the reports coming in
earlier years.
Professional indoor tanning salons understand that it is inappropriate
to make direct
health claims about indoor tanning or to suggest there are no risks
associated with
UV exposure from any source. But regardless of what a facility can say
about its services,
surveys show many indoor tanners utilize tanning for more than just the
cosmetic tan.
Tanning: Nature’s Sunscreen
One reason so many people enjoy the professional indoor tanning
experience is
that trained operators can give a tanner controlled UV exposures to
gradually
develop natural sunscreen – often called a "base tan" – while minimizing
the risk of sunburn.
The tanning process actually creates two different forms of natural
protection against sunburn:
Melanin pigment produced when UV light meets the skin literally
enshrouds and
shields skin cells in the skin’s epidermis, protecting each cell from
getting too much UV exposure. Melanin is a powerful anti-oxidant,
helping the skin naturally eliminate
free-radicals that can cause damage.
As the skin tans, the outer layer thickens (a natural process called
acanthosis)
which is nature’s design to make the skin naturally more resistant to
sunburn.
The value of a base tan, as any indoor tanner knows, is that it adds
another layer to your sun protection arsenal – making sunscreen worn
outdoors for outings on sunny
days even more effective. Here’s how that works:
A typical new client begins tanning with 5-minute sessions, gradually
develops a
tan and can work her/his way up to 20-minute sessions. At this point,
she/he
becomes naturally FOUR TIMES more resilient to sunburn than when she/he
first
started tanning. (5 minutes x 4 = 20 minutes). So that tan has an SPF 4
value.
When someone with a base tan uses sunscreen outdoors, they essentially
multiply
the effectiveness of the sunscreen. In other words, an SPF 15 product
applied to
the skin of a person whose base tan has already made her four times more
resilient
to sunburn creates a net SPF of 60. (SPF 15 x 4 = SPF 60).
In sunny environments many fair-skinned people can sunburn during normal
outdoor activities even while wearing sunscreen. But with a base tan
their sunscreen
becomes more effective and they are much less likely to sunburn.

Casual Self-Treatment of Cosmetic Skin Conditions
Millions of indoor tanning customers frequent U.S. indoor tanning salons
for
their own self-treatment of cosmetic skin conditions and other
non-cosmetic
tanning reasons - physiologic benefits that can occur when one follows
the cosmetic
regimen at a tanning facility. According to a 2010 Smart Tan survey:
More than three million consumers frequent tanning salons for
self-treatment of psoriasis, eczema, acne, vitiligo, seasonal affective
disorder (SAD) and to increase vitamin D levels.
Approximately one million indoor tanners said they were referred to
tanning
facilities by their dermatologist.
Could Indoor Tanning Be a Surrogate for What Nature Intended?
Vitamin D production is one of the benefits that has been associated
with human
exposure to ultraviolet-B (UVB) emitted in sunlight and by an estimated
90 percent of commercial indoor tanning equipment. While the North
American indoor tanning industry conducts indoor tanning as a cosmetic
service, an undeniable physiological side effect of this service is that
indoor tanning clients manufacture sufficient levels of
vitamin D as a result of indoor tanning sessions.
Vitamin D is a hormone produced naturally when skin is exposed to UVB in
sunlight or indoor tanning units. Scientists through thousands of
studies now recommend
vitamin D blood levels of 40-60 ng/ml. Only those who get regular
UV exposure have those levels naturally:
Indoor Tanners...........................42-49 ng/ml...........................Sufficient
Non-Tanners................................23-25 ng/ml...........................Deficient
Dermatologists...........................13-14 ng/ml...........................Severe
Deficiency
Vitamin D sufficiency is linked to a reduction in 105 diseases,
including heart disease,
diabetes, multiple sclerosis and most forms of cancer. It is believed
that vitamin D
deficiency contributes to nearly 400,000 premature deaths and adds a
$100 billion burden
to our health care system.
77 percent of Americans are considered vitamin D deficient according to
government
data and overzealous sun avoidance is the only plausible explanation for
the
50 percent increase in that figure in the past 15 years.
The indoor tanning industry believes that, for those individuals who can
develop tans,
the cosmetic and vitamin D-related benefits of non-burning exposure to
ultraviolet light
in appropriate moderation outweigh the easily manageable risks
associated with overexposure and sunburn. Many doctors agree: "I believe
the health benefits of exposure to UVA and
UVB rays greatly outweigh the disadvantages, even if that means using a
sunbed
during winter months." -British Oncologist Dr. Tim Oliver -
885 Woodstock Road, Suite 205
Roswell GA 30075
Store hours:
Monday - Thursday 10am - 8pm
Friday - Saturday 10am - 7pm
Sunday 11am - 5pm
After hours call: 404-405-4069